Ovarian Cancer Diagnosis through White Blood Cell Count Examinations
Ovarian cancer is a serious condition that occurs when ovarian cells grow abnormally. While blood tests and white blood cell counts can provide valuable insights, they are not generally reliable for diagnosing ovarian cancer.
Doctors can use various imaging techniques such as MRI scans, ultrasounds, and CT scans to detect abnormal masses around the pelvis. However, these scans cannot differentiate between tumors and other abnormal masses, and they are still helpful in the early stages of diagnosis and for monitoring the growth or spread of tumors.
A biopsy is necessary for an accurate ovarian cancer diagnosis. Surgeons may remove an entire tumor for testing during a biopsy, or a smaller sample may be collected using a very fine needle. Ultrasound-Guided Tru-Cut Biopsy, in particular, provides reliable histological confirmation of malignancy and helps identify cancer subtypes important for treatment planning.
Beyond imaging and biopsy, alternative diagnostic tools include molecular and genetic testing such as next-generation sequencing (NGS) on tumor tissue. This helps identify inherited cancer risks and offers greater specificity than traditional blood tests. Liquid Biopsy Approaches, analyzing cell-free DNA (cfDNA) fragmentomes from blood samples combined with protein biomarkers like CA-125 and HE4, aim to improve early-stage detection by identifying cancer-specific genetic and epigenetic changes in circulating DNA fragments.
CA-125 tests are used to monitor treatment progress for ovarian cancer and to check whether cancer has returned after treatment. However, it's important to note that several other conditions can cause spikes in CA-125 levels, making it an unreliable diagnostic tool for ovarian cancer.
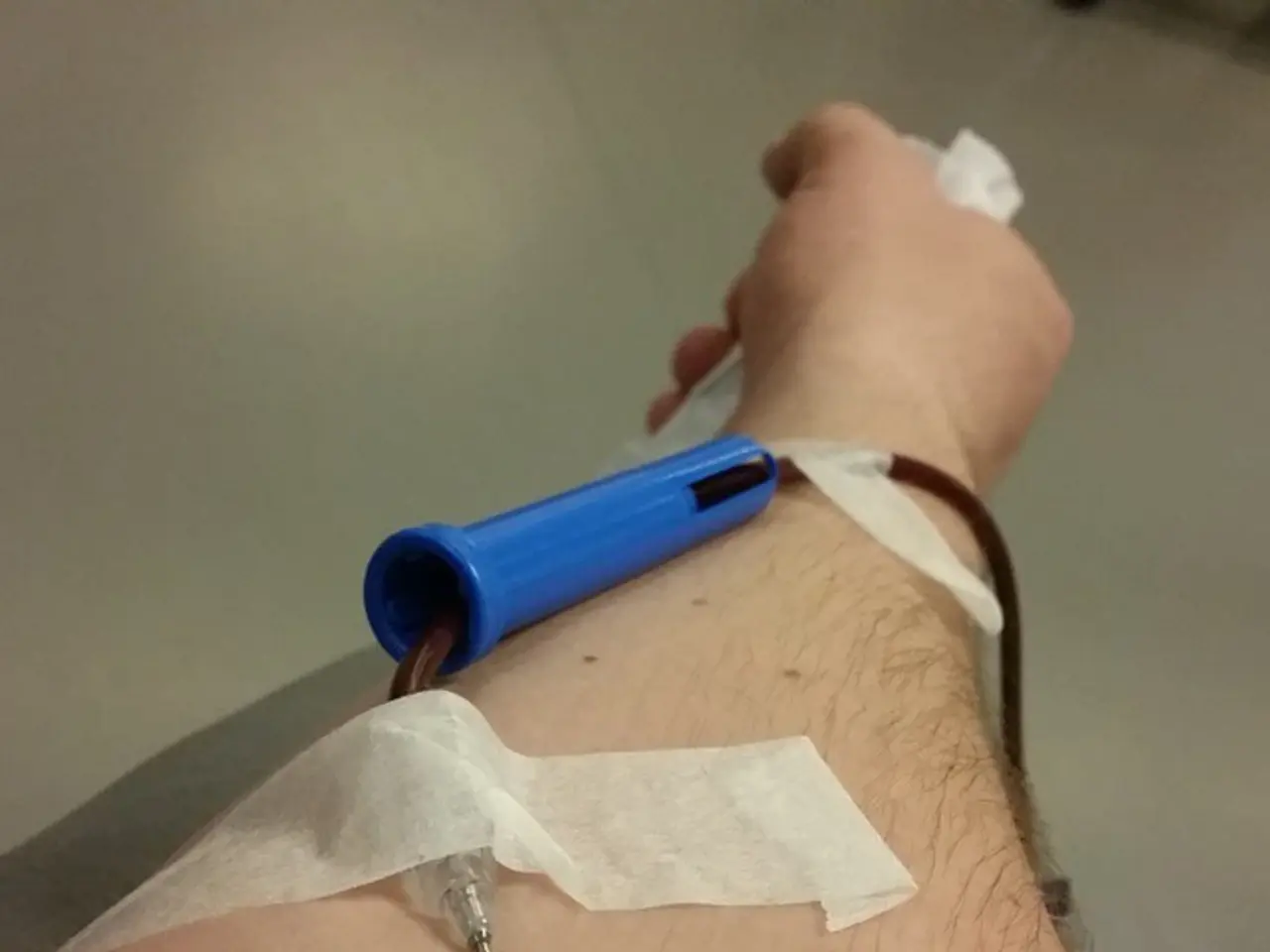
White blood cell levels can provide doctors with insights into a person's overall health. In people with certain cancers, such as leukemia, white blood cell levels can be elevated. Common side effects of white blood cell counts include bruising, bleeding, and swelling around the needle entry site. Some people may also become faint or dizzy during the test.
Urea and electrolyte tests allow doctors to determine if a person's kidneys are functioning correctly. Abnormal levels of waste chemicals or electrolytes in these tests may indicate kidney disease, heart disease, dehydration, or diabetes.
In conclusion, a combination of imaging, biopsy, molecular profiling, and advanced liquid biopsy techniques form the core of alternative diagnostic tools for ovarian cancer. These methods provide more specific, sensitive, and early detection capabilities essential for accurate diagnosis and treatment planning.
- Ovarian cancer is a serious medical condition, and while blood tests and white blood cell counts can offer insights, they are not generally reliable for diagnosing ovarian cancer.
- Beyond imaging and biopsy, molecular and genetic testing, such as next-generation sequencing (NGS) on tumor tissue, can help identify inherited cancer risks and offer greater specificity than traditional blood tests.
- CA-125 tests are used to monitor treatment progress for ovarian cancer and to check whether cancer has returned after treatment, but it's important to note that several other conditions can cause spikes in CA-125 levels, making it an unreliable diagnostic tool for ovarian cancer.
- Urea and electrolyte tests are vital in determining kidney function and can indicate kidney disease, heart disease, dehydration, or diabetes, which are all important health-and-wellness concerns, especially in women's health.