Emergency room visit for a charred infant in California results in financial chaos for the family, facing a staggering bill of $100,000.
In a troubling case that highlights gaps in the implementation and practices of insurance companies, a California family faced steep bills for emergency air transport services despite legal protections.
Jessica Farwell's insurance covered less than half of the $90,000 helicopter bill because the air ambulance service charged much more than what her insurance considered usual or reasonable rates. This left her responsible for a large surprise balance—about $57,929.80—after insurance reimbursement.
Despite doctors' assurances she wouldn’t be charged, her insurer only covered part of the helicopter and ambulance fees, and the remaining high charges were passed on to her. This is a common issue with emergency air transport billing in the U.S.
Regarding California law AB 716, it was enacted to address surprise medical billing for emergency services, including air ambulance rides. This law requires insurers and providers to resolve payment disputes through a state-administered independent dispute resolution process, protecting patients from excessive out-of-pocket costs for emergency care received out-of-network. AB 716 aims to prevent situations like Farwell’s by capping patient liability and eliminating surprise bills from emergency and air ambulance services, though enforcement and insurer compliance are ongoing challenges.
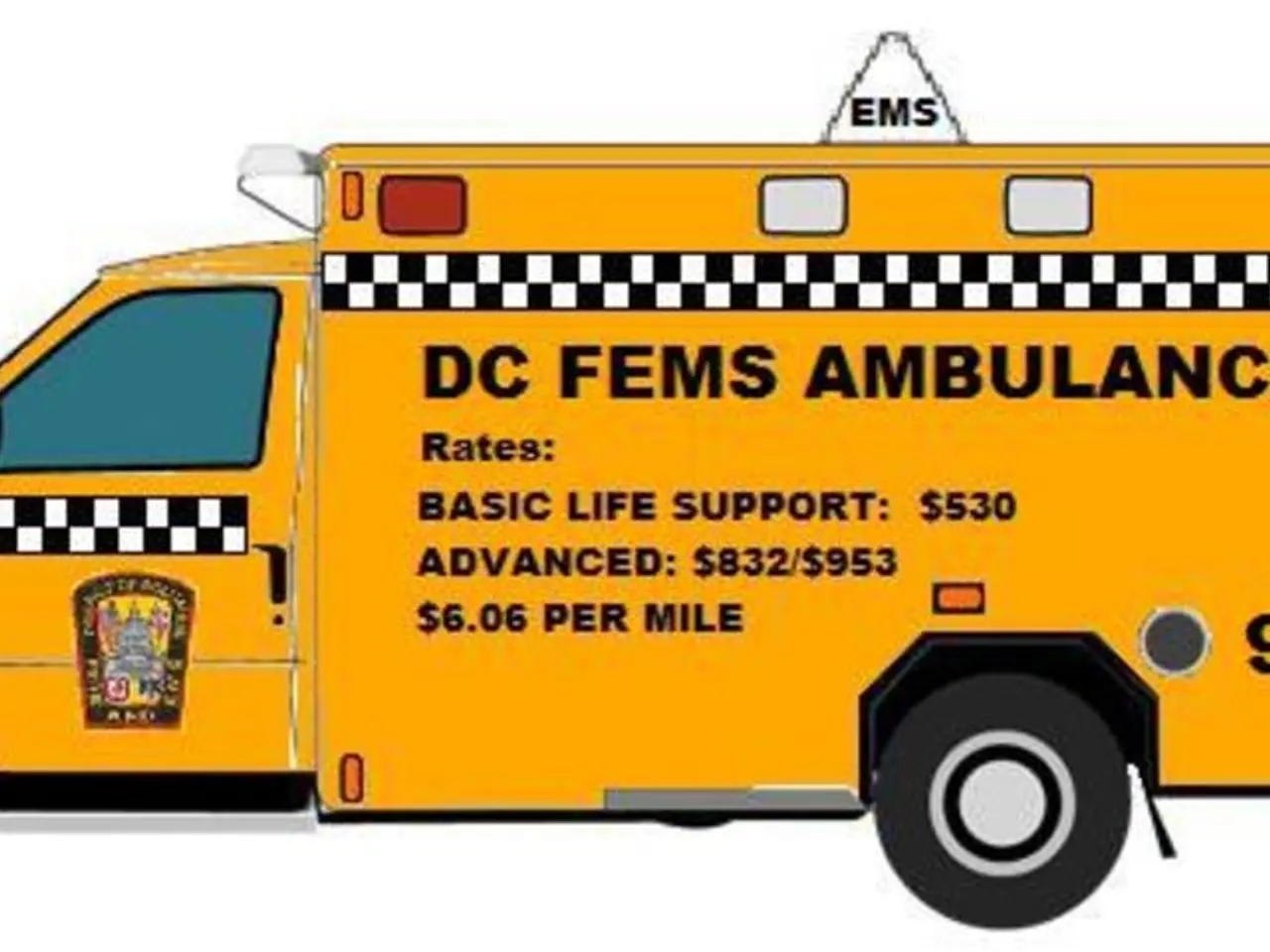
The incident that led to Farwell's ambulance ride involved her newborn baby, Brody, who suffered severe burns from a rice cooker falling off a kitchen counter. Doctors deemed it medically necessary to transfer Brody to Shriners Children's Hospital in Sacramento. The nearest hospital did not have a burn unit or any ambulances available, forcing the family to take a $90,000 air ambulance for a 15-minute ride to the hospital. Upon arrival at the helipad, the family was required to take another ambulance ride, which was 0.3 miles to the hospital entrance, costing $10,200.
The family received bills totaling more than $100,000 for the 15-minute helicopter ride and the 0.3-mile ambulance ride. The incident took place shortly after Farwell left her job to care for her children. As a result, she was left struggling with the bills, receiving constant calls from collection companies.
However, after the ABC San Francisco affiliate KGO's intervention, the $100,032 bills for the helicopter and ambulance rides were waived.
This case underscores the need for improved enforcement and compliance with laws like AB 716 to protect consumers from unexpected and exorbitant medical bills in emergency situations.
- Advocacy for strengthened enforcement and compliance with California law AB 716 is crucial, as it aims to prevent cases like Jessica Farwell's, where medical-conditions necessitated an emergency air transport, yet she was saddled with exorbitant bills due to insurance disputes and unexpected out-of-pocket expenses.
- Despite Brody Farwell's medical transportation costs being covered under health-and-wellness insurance, the family was still faced with a substantial balance because the air ambulance service charged rates deemed unreasonable by the insurance company, highlighting the need for transparency and regulation in the medical and science industries regarding emergency air transport services.